Customer success
Headlamp streamlines data collection so Dr. Faherty can spend each visit on meaningful discussion and decision-making.
Behavioral and physiological trends reveal insights traditional records often miss.
Headlamp helps family physicians bridge the gap between mental and physical health for a fuller picture of patient well-being.

“I used to think I had to rely on what patients could recall. But when you can see their patterns in context, you realize how much you were missing.”
Results: Seeing What Labs Cannot
With decades of experience in family medicine, Dr. Faherty has worked with nearly every type of health record and monitoring tool available. He chooses Headlamp because it captures what those systems cannot: how patients actually live, sleep, and recover between visits. By visualizing behavioral patterns such as sleep quality, daylight exposure, activity, and mood alongside clinical data, he gains a clearer view of the whole person, not just their test results.
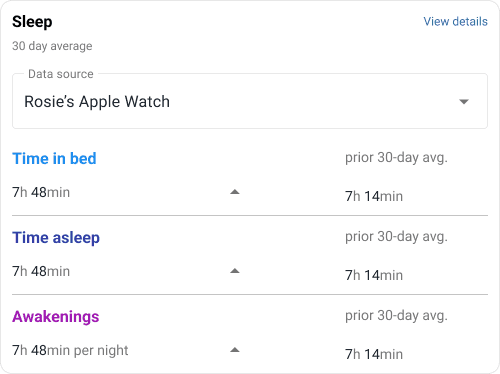
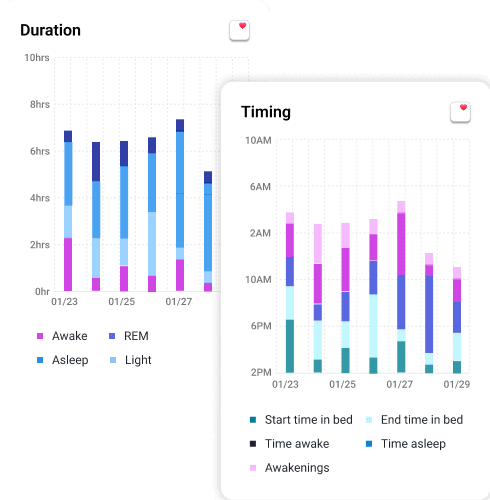
Much of this context comes from passive data collection through connected devices and phone sensors, giving him continuous insight without adding new steps for patients. For complex or chronic cases, these trends often reveal root causes that routine testing misses. A patient who reports “sleeping fine” might still show dozens of nightly awakenings, or their daylight exposure might drop before mood changes appear.
Having this information ready before each visit allows Dr. Faherty to focus on what matters most: education, reassurance, and long-term planning. Patients leave each appointment feeling understood and involved in their progress, seeing patterns that help their experience make sense.
“I used to think I had to rely on what patients could recall. But when you can see their patterns in context, you realize how much you were missing.”
One of Dr. Faherty’s longtime patients had been treated for bipolar II disorder since 2019. Despite several medication adjustments, her mood instability continued. She was using standard mood-stabilizing treatments but relied on as-needed medications for anxiety and irritability.
“She was certainly frustrated,” Dr. Faherty recalls. “It felt like we were both stuck, doing everything right on paper but getting nowhere.”
Her swings into hypomania, but primarily depression, were less severe yet still far from manageable. Anxiety was unpredictable and exhausting, often flaring without clear cause. Each episode left her discouraged, cycling through hope and disappointment as months went by. She felt trapped in a pattern of symptom management, not healing, returning every three months for the same conversation and the same uncertainty despite counseling and medication adherence.
“She was certainly frustrated,” Dr. Faherty recalls. “It felt like we were both stuck, doing everything right on paper but getting nowhere.”
“The data told a story I would have missed. Once we treated her sleep apnea, her bipolar symptoms improved dramatically.”
The sleep-apnea discovery changed more than one life. It reshaped how Dr. Faherty approaches every visit. He now scans behavioral patterns as a routine part of chronic care, whether he is helping teens manage anxiety, adults navigate trauma, or older patients balance multiple conditions.
“Headlamp tells a story. It helps me see the person behind the symptoms.”
Headlamp has become a bridge between experience and evidence. It helps him validate what patients feel and uncover what might be driving those feelings. In many cases, it has prevented unnecessary medication changes and strengthened trust by showing patients that their concerns have measurable context.
“I want patients to leave knowing we are on the same side. Headlamp gives us both a clearer view of what is really happening.”
Time that once went into paperwork now goes toward richer conversations and clearer decisions. For Dr. Faherty, that is the true benefit: deeper connection and more effective care.
Ready to Practice Psychiatry Your Way?
See how Headlamp Health helps clinicians reclaim time, make informed decisions, and build sustainable, patient-centered practices.