Customer success
Identified an underlying ADHD diagnosis that had been masked by anxiety through Headlamp’s mood descriptors and longitudinal data.
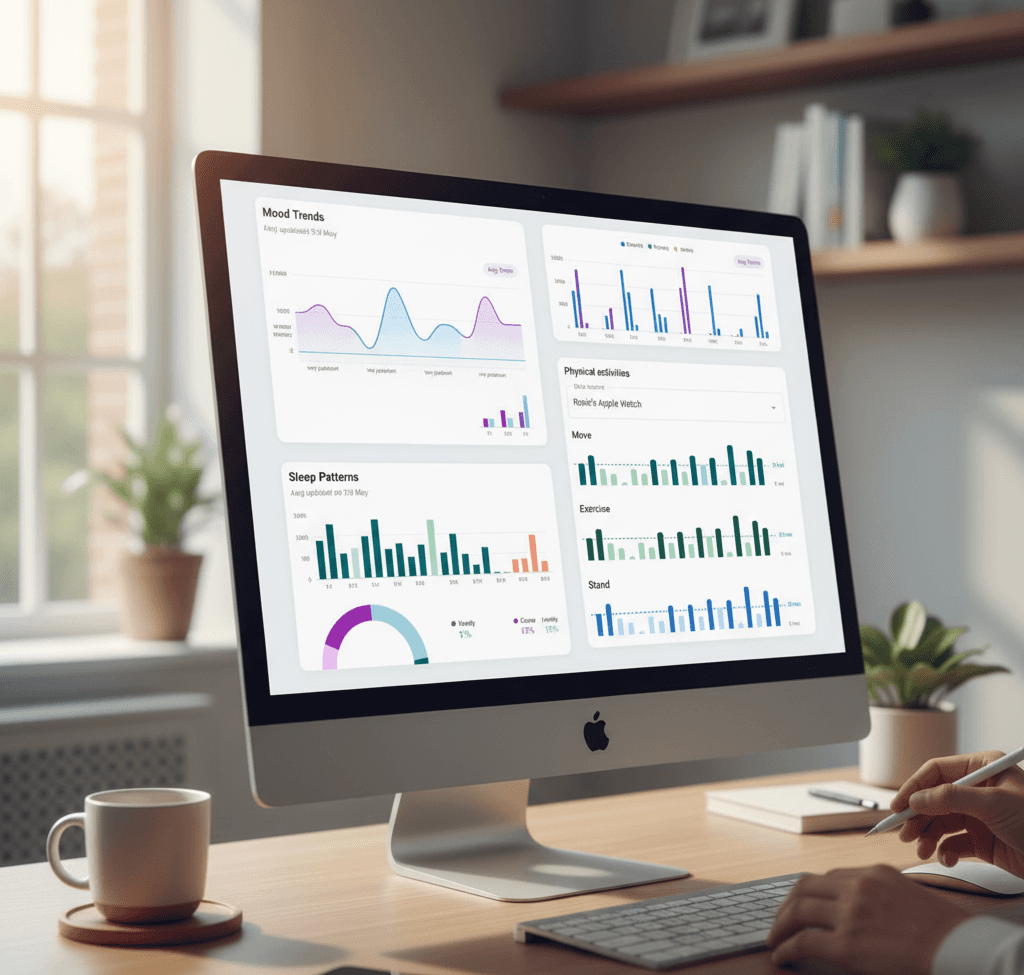
Reviews Headlamp data before and during each session, turning intake time into deeper, more informed discussion.insights traditional records often miss.
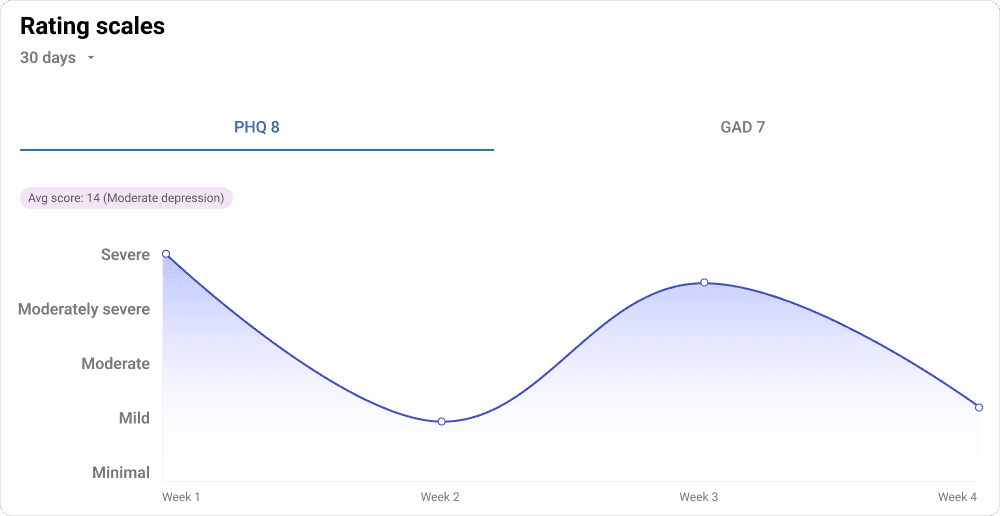
Patient PHQ-9 scores in Headlamp reflected 55% greater symptom severity than office assessments, giving Nichole a clearer picture of true patient need.
“I wanted no limitations in how I treated my patients. I wanted the freedom to give them the time and attention they deserve and to truly put them first.”
Results: Seeing What Labs Cannot
With over 20 years of medical experience, Psychiatric Nurse Practitioner Nichole McLeod uses Headlamp Health to look past surface symptoms and understand the full story behind each patient’s mental health.
Nichole began her career as an emergency room nurse, working long shifts filled with noise, urgency, and fluorescent light. The ER taught her to think fast, but it also showed her how easily people in emotional distress can be treated as problems to manage rather than individuals to understand. That experience shaped the way she practices today.
After years in larger, insurance-based systems, Nichole joined Lavender Psychiatry, where she began building long-term therapeutic relationships that reaffirmed her philosophy: care takes time. When she decided to open her own practice, she wanted to keep that same human-centered model while working more efficiently and independently.
“Nothing matters more than listening to the patient and understanding where they’re coming from,” she says. “Sometimes they don’t even know where they want to go, but they know that where they are isn’t enough.”
Before using Headlamp Health, Nichole began each session the same way many clinicians do. She asked a long list of questions to rebuild the patient’s story from memory. How had they slept? What had their energy been like? When did their mood start to dip? Each appointment began with data collection before she could move into the insight and understanding that actually drive change.
“I was spending so much time trying to get to the starting line,” she says. “It is hard to build momentum when you are always catching up.”
Now, Nichole begins each appointment with a clear picture already in view. She opens Headlamp on her iPad, reviews the patient’s recent check-ins, and notes changes in mood, sleep, or energy levels. The information is available in real time, ready to guide the session.
In one case, a patient came in reporting anxiety and panic attacks. At first, it appeared straightforward. But when Nichole reviewed the patient’s Headlamp data, she noticed recurring words like “disorganized,” “scattered,” and “indifferent.” Those trends suggested something different.
“They were not anxiety words,” she says. “They pointed toward ADHD and depression.”
She adjusted her questions to explore focus, organization, and daily routines. The patient revealed that they often lost track of tasks and felt frustrated by their own disorganization. By the end of the visit, Nichole had updated the diagnosis and treatment plan to reflect the true cause.
“Without those descriptors, I probably would have kept treating anxiety,” she says. “But when I looked at the data, I could see the real pattern. It changed my questions and the entire treatment plan.”
What used to take multiple sessions now happens within one. The difference is not about speed, but about precision. Nichole starts each appointment with understanding instead of assumption.
Before using Headlamp Health, Nichole began each session the same way many clinicians do. She asked a long list of questions to rebuild the patient’s story from memory. How had they slept? What had their energy been like? When did their mood start to dip? Each appointment began with data collection before she could move into the insight and understanding that actually drive change.
Before each appointment, she glances at the patient’s recent entries to orient herself. During the session, she often invites the patient to look at the screen with her. Together, they scroll through charts and descriptors and discuss what stands out.
“I will ask, ‘Tell me more about why you picked this mood that day,’” she says. “It helps the patient connect the dots themselves.”
That collaboration turns abstract experiences into something visible. A patient might notice that their energy dips every Sunday evening or that poor sleep precedes a low mood. Nichole uses those discoveries to guide treatment decisions, from adjusting medication to suggesting behavioral changes.
She also uses Headlamp’s integrated lab and medication data to identify possible medical contributors to mood or fatigue. “I can look at lab results, see when they were done, and check if the patient is being treated,” she says
“If everything looks normal but they are still exhausted, I know it is time to look closer at depression or another cause.”
The result is a process that feels personal rather than procedural.
“Headlamp does not replace the relationship,” she says. “It strengthens it. I can listen more deeply because I already see where to start.”
Since bringing Headlamp into her practice, Nichole says her sessions feel more focused and meaningful. “I changed a treatment plan today because of what I saw in Headlamp,” she says.
“The patient left feeling understood, like this was the first time someone truly saw what was going on.”
Her patients notice the difference. They no longer feel like they are starting from scratch at every visit. Instead, they see their own progress and patterns on the screen, which helps them feel validated and more engaged in their care.
“My patients can see their story on the screen,” she says. “That is powerful. It makes them feel like part of their care instead of a subject of it.”
The improvement extends to measurable outcomes as well. In one case, a patient’s PHQ-9 score during an in-office screening was 9. A week later, their Headlamp submission showed a score of 14, revealing more severe symptoms that required a different approach.
“It showed me that timing matters,” she says. “A patient’s day, their stress, even when they take the survey, all of that shapes what we see. Headlamp gives me a more honest picture.”
Ready to Practice Psychiatry Your Way?
See how Headlamp Health helps clinicians reclaim time, make informed decisions, and build sustainable, patient-centered practices.